Key facts
- Influenza is an acute viral infection that spreads easily from person to person.
- Influenza circulates worldwide and can affect anybody in any age group.
- Influenza causes annual epidemics that peak during winter in temperate regions.
- Influenza is a serious public health problem that causes severe illnesses and deaths for higher risk populations.
- An epidemic can take an economic toll through lost workforce productivity, and strain health services.
- Vaccination is the most effective way to prevent infection.
Overview
Seasonal influenza is an acute viral infection caused by an influenza virus.
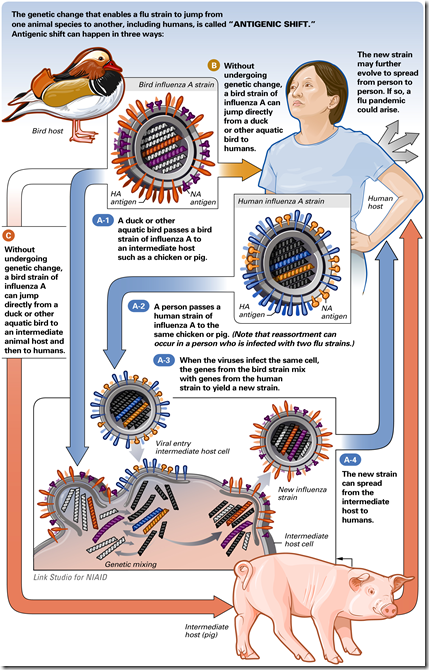
There are three types of seasonal influenza – A, B and C. Type A influenza viruses are further typed into subtypes according to different kinds and combinations of virus surface proteins. Among many subtypes of influenza A viruses, currently influenza A(H1N1) and A(H3N2) subtypes are circulating among humans. Influenza viruses circulate in every part of the world. Type C influenza cases occur much less frequently than A and B. That is why only influenza A and B viruses are included in seasonal influenza vaccines.
Signs and symptoms
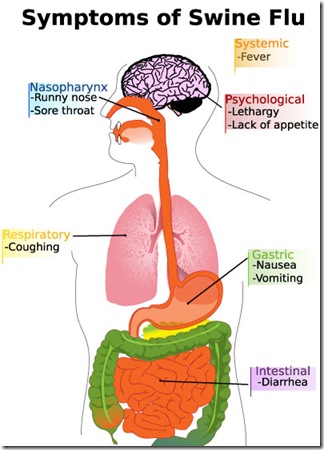
Seasonal influenza is characterized by a sudden onset of high fever, cough (usually dry), headache, muscle and joint pain, severe malaise (feeling unwell), sore throat and runny nose. Most people recover from fever and other symptoms within a week without requiring medical attention. But influenza can cause severe illness or death in people at high risk (see below). The time from infection to illness, known as the incubation period, is about two days.
Who is at risk?
Yearly influenza epidemics can seriously affect all age groups, but the highest risk of complications occur among children younger than age two, adults age 65 or older, and people of any age with certain medical conditions, such as chronic heart, lung, kidney, liver, blood or metabolic diseases (such as diabetes), or weakened immune systems.
Transmission
Seasonal influenza spreads easily and can sweep through schools, nursing homes or businesses and towns. When an infected person coughs, infected droplets get into the air and another person can breath them in and be exposed. The virus can also be spread by hands infected with the virus. To prevent transmission, people should cover their mouth and nose with a tissue when coughing, and wash their hands regularly.
Treatment
Antiviral drugs for influenza are available in some countries and effectively prevent and treat the illness. There are two classes of such medicines, 1) adamantanes (amantadine and remantadine), and 2) inhibitors of influenza neuraminidase (oseltamivir and zanamivir). Some influenza viruses develop resistance to the antiviral medicines, limiting the effectiveness of treatment. WHO monitors antiviral susceptibility in the circulating influenza viruses.
Seasonal epidemics
Influenza epidemics occur yearly during autumn and winter in temperate regions. Illnesses result in hospitalizations and deaths mainly among high-risk groups (the very young, elderly or chronically ill). Worldwide, these annual epidemics result in about three to five million cases of severe illness, and about 250 000 to 500 000 deaths. Most deaths associated with influenza in industrialized countries occur among people age 65 or older. In some tropical countries, influenza viruses circulate throughout the year with one or two peaks during rainy seasons.
Disease effects
Influenza can cause serious public health and economic problems. In developed countries, epidemics can result in high levels of worker absenteeism and productivity losses. In communities, clinics and hospitals can be overwhelmed when large numbers of sick people appear for treatment during peak illness periods. While most people recover from a bout of influenza, there are large numbers of people who need hospital treatment and many who die from the disease every year. Little is known about the effects of influenza epidemics in developing countries.
Prevention
The most effective way to prevent the disease or severe outcomes from the illness is vaccination. Safe and effective vaccines have been available and used for more than 60 years. Among healthy adults, influenza vaccine can prevent 70% to 90% of influenza-specific illness. Among the elderly, the vaccine reduces severe illnesses and complications by up to 60%, and deaths by 80%.
Vaccination is especially important for people at higher risk of serious influenza complications, and for people who live with or care for high risk individuals.
WHO recommends annual vaccination for (in order of priority):
- nursing-home residents (the elderly or disabled)
- elderly individuals
- people with chronic medical conditions
- other groups such as pregnant women, health care workers, those with essential functions in society, as well as children from ages six months to two years.
Influenza vaccination is most effective when circulating viruses are well-matched with vaccine viruses. Influenza viruses are constantly changing, and the WHO Global Influenza Surveillance Network (GISN), a partnership of National Influenza Centres around the world, monitors the influenza viruses circulating in humans. WHO annually recommends a vaccine composition that targets the three most representative strains in circulation.